Vitals
Signs from the Schools
School of Health Professions
School of Nursing
School of Medicine
Graudate School of Biomedical Sciences
Jerry H. Hodge School of Pharmacy
School of Health Professions
Hear Me Out, CARL
 For audiology students in the School of Health Professions, one of the most skills
to master is fitting patients for hearing aids. The procedure requires inserting a
probe into the ear canal, which allows clinicians to identify the correct sized hearing
aid. CARL (Canadian Audiology simulator for Research and Learning) is a 3-D printed
manikin simulator used to teach students probe placement. He makes his debut this
year with 12 Doctor of Audiology students.
For audiology students in the School of Health Professions, one of the most skills
to master is fitting patients for hearing aids. The procedure requires inserting a
probe into the ear canal, which allows clinicians to identify the correct sized hearing
aid. CARL (Canadian Audiology simulator for Research and Learning) is a 3-D printed
manikin simulator used to teach students probe placement. He makes his debut this
year with 12 Doctor of Audiology students.
EARS
CARL’s ears are silicone and modeled from human CT scan imagery, creating anatomically
correct ears.
CAMERA
This tiny camera produces images on the computer screen of CARL’s ear canal, allowing
the student to visualize the probe.
PROBE
These are inserted in the ear before the molding material is inserted in the ear canal.
SOFTWARE
Students see in real-time how they are inserting the probe, providing instant feedback.
The software includes modules for practice and testing and can simulate different
levels of hearing loss, information needed to properly fit a hearing aid.
Trapped Inside Her Brain
On a Sunday night in 2016, Ninfa Flores was getting ready for the upcoming work week. She had an early start on Monday morning in the Texas Tech University Services Operations Division. Flores had spent 39 years in the department working up to her current position of assistant director and was proud of how far she’d come. On Monday morning, however, Flores never showed up for work.
 She’d had a stroke Sunday night. Her entire left side was weakened, and her left hand
(her dominant hand) was later broken. The rest of her was trapped inside her brain.
Flores couldn’t remember things and couldn’t communicate her thoughts. Her identity
that she’d worked so hard to create came crashing down. Doctors advised her to retire,
and even though she wasn’t ready, she was forced to confront the fact that she could
no longer handle the work responsibilities. She gave up her job and her ability to
interact with other people at the same time. The woman who had worked under five different
chancellors at TTU had aphasia.
She’d had a stroke Sunday night. Her entire left side was weakened, and her left hand
(her dominant hand) was later broken. The rest of her was trapped inside her brain.
Flores couldn’t remember things and couldn’t communicate her thoughts. Her identity
that she’d worked so hard to create came crashing down. Doctors advised her to retire,
and even though she wasn’t ready, she was forced to confront the fact that she could
no longer handle the work responsibilities. She gave up her job and her ability to
interact with other people at the same time. The woman who had worked under five different
chancellors at TTU had aphasia.
“I didn’t want to go out and talk to people — I no longer had the confidence and was scared to try,” Flores said.
Her home health therapist noticed her despair and told her about the Stroke & Aphasia Recovery (STAR) Program offered at the TTUHSC School of Health Professions in the Department of Speech, Language and Hearing Sciences.
“When I had my stroke, my sister got sick and ended up in the hospital, too. She was at UMC and I was at Covenant. My daddy said, ‘I didn’t raise my girls to be quitters,’” Flores said. “This gave me the motivation to try.”
She began attending the Tuesday morning STAR Program therapy sessions, where she met other stroke survivors – many just like her. “Todd in my group really motivated me to try because when I first came, he couldn’t write either, but then he started writing a full page! Now, I can write my initials,” Flores said proudly.
Flores also participated in the STAR Program Summer Arts Camp — a two-week program — and learned how to paint with her right hand. She loves the beach and painted scenes from South Padre Island and the Dominican Republic. The Texas Tech University Public Art Program invited STAR Program members to showcase their art in the Texas Tech University System building and Flores is excited to see her paintings displayed there — in a building she’s very familiar with since she used to supervise the cleaning of it.
I Can't Even Describe How it Felt
Maria Drews, DPT, (Health Professions, ’18) walked into the living room and noticed swelling in her 9-month-old son’s right temple. Of course, she took him to his pediatrician, as a precaution, and was told to observe it for any changes.
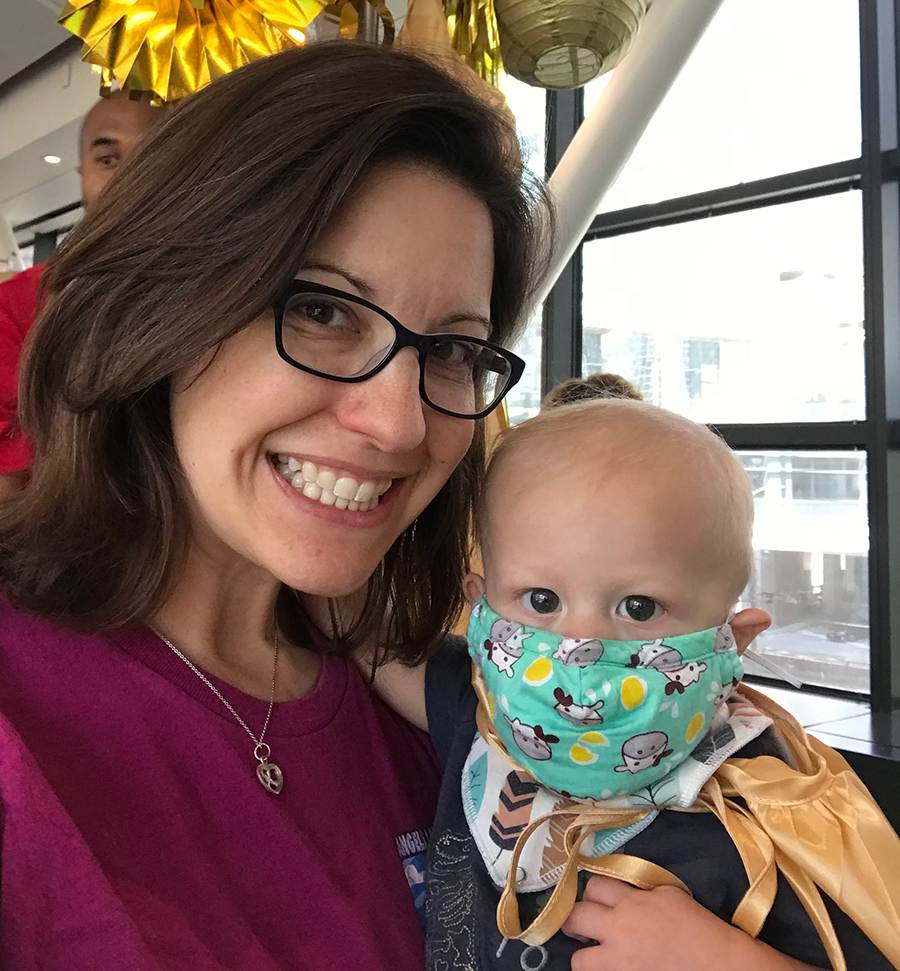 Two weeks later, “It’s now the size of a quarter, and it’s hard,” Drews told the pediatrician
during a phone call. The physician referred her son, Lucas, to a plastic surgeon for
an ultrasound and X-ray, which provided inconclusive results; an MRI and biopsy were
needed. In the two and a half weeks it took to schedule the MRI, Lucas developed a
high fever, forcing Drews and her husband to take him to the emergency room. Blood
work revealed an alarming elevation in his white blood cell count. Lucas’ fever would
respond to medication, but it never completely broke. They went back to the pediatrician
who referred them to an ear, nose and throat specialist — still no results.
Two weeks later, “It’s now the size of a quarter, and it’s hard,” Drews told the pediatrician
during a phone call. The physician referred her son, Lucas, to a plastic surgeon for
an ultrasound and X-ray, which provided inconclusive results; an MRI and biopsy were
needed. In the two and a half weeks it took to schedule the MRI, Lucas developed a
high fever, forcing Drews and her husband to take him to the emergency room. Blood
work revealed an alarming elevation in his white blood cell count. Lucas’ fever would
respond to medication, but it never completely broke. They went back to the pediatrician
who referred them to an ear, nose and throat specialist — still no results.
No one had an answer.
Finally, the time had come for the MRI, which Lucas underwent with a fever. The doctors discovered the mass was retreating from the outer edge of the skull toward the brain — Lucas’ pediatrician wanted him to be admitted overnight for monitoring. While Maria fills out the admission paperwork, she sees a wall of doctors coming into Lucas’s room, one of them mentioning leukemia.
Another MRI was ordered with an oncologist confirming the diagnosis on May 1, 2018: Lucas had acute myeloid leukemia (AML-M7) — a rare form of leukemia most commonly found in children with Down syndrome. The mass on his head that originally caught Drews’ attention was a chloroma: a collection of leukemic cells occurring outside the bone marrow.
Lucas’ diagnosis naturally put the brakes on some of Maria’s plans. She had completed her DPT degree with TTUHSC in December 2018 with plans to participate in the May 2019 graduation. She called her adviser to explain why she wouldn’t be at the graduation ceremony, then thought nothing more about it as she juggled her full-time job and Lucas’ chemotherapy appointments. Then something unexpected happened.
A few weeks later, Drews received an email from gift officer Cliff Wilkes asking if the School of Health Professions could bring the graduation to her. “I just didn’t understand — it was so amazing,” she recalled. When she saw Dean Lori Rice Spearman, PhD, (Biomedical Sciences ’86) — now TTUHSC provost and chief academic officer — coming toward her with regalia and a diploma, the emotion overwhelmed her. In the hallway of her workplace, Drews received her diploma. “My journey, my education, my baby boy’s survival was important to my school … I can’t even describe how that felt, not only to me, but my friends, family and co-workers. I mean, who does that?”
Lucas received a bone marrow transplant on Oct. 17, 2019, and is now in remission.
School of Nursing
Cheerleader Flips into Nursing School
Q. How did you first become involved in cheerleading?
A. I had a couple of friends, at Downers Grove South High School in Chicago,  Illinois, who were looking for a guy to be on their cheer team. Our high school had
a coed team, and they knew that I used to be a hip-hop dancer, so they thought I’d
be pretty good at it. So, I just said why not, and I tried out for the team.
Illinois, who were looking for a guy to be on their cheer team. Our high school had
a coed team, and they knew that I used to be a hip-hop dancer, so they thought I’d
be pretty good at it. So, I just said why not, and I tried out for the team.
Q. How did you become interested in nursing?
A. I knew I wanted to do something with the medical field. I actually started working
as a transport aid at UMC Health System to get some medical experience. As I was working,
I noticed how hard-working, ethical and empathetic the nurses were. I talked to them
a lot throughout my shifts over the next year and a half. From there I just loved
the nurses at UMC, and wanted to strive to be just like them.
Q. What nursing school program are you in?
A. I am in level one of the Traditional BSN program.
Q. What type of nurse do you want to become and why?
A. My main goal would be to become a cardiac intensive care unit nurse for a couple
of years and then the ultimate goal would be a travel nurse while I’m still young
and don’t have any full commitments.
Q. How has cheerleading prepared you for nursing school?
A. It has taught me not to give up. Coming to college in Texas, I wasn’t an amazing
cheerleader, but I went through a lot of obstacles mentally Q. and physically throughout
my career. I knew if I started something, I would not give up and stop halfway through.
School of Medicine
Not All Bacteria Are Created Equal
Researchers use probiotics on opportunistic pathogens
The human microbiome is complex and research is ongoing on the effects of probiotics in everyday health. TTUHSC researchers may have found a novel use for these live bacteria: to fight infectious bacteria in burn patients. “The opportunistic pathogen Psudomonas aeruginosa grows in the burn wound and then spreads within the body of the burned patient, leading to sepsis,” said Abdul Hamood, PhD, a professor in the School of Medicine Department of Immunology and Molecular Microbiology. To make things more complicated, this pathogen is antibiotic resistant. To prevent the infection from occurring, Hamood and his team are using probiotics.
The study, “Application of Lactobacillus Gasseri 63 AM Supernatant to Pseudomonas aeruginosa- Infected Wounds Prevents Sepsis in Murine Models of Thermal Injury and Dorsal Excision,” was published in the August 2019 issue of the Journal of Medical Microbiology.
The Free Clinic Turns 10
The Free Clinic opened its doors in 2009 and is a student-run facility for the uninsured citizens of Lubbock County. Operation hours are from 6 p.m. to 10 p.m. every Wednesday night at the Lubbock Impact community outreach facility.
The Clinic:
Total patient visits (2009-2019):
13,000
Total volunteers (2009-2019):
1,500 medical students
450 faculty members
Total exam rooms: 14
Up to 30 patients seen each Wednesday night
The Service Area:
More than 18% of the Lubbock population is uninsured
22.5% of the Lubbock population is below the national poverty line
Are You Sure You Have the Right Person?
Meredith Gavin, fourth-year medical student, couldn’t believe she’d won the  2019 TTUHSC Clinical Research Institute Medical Student Award for Outstanding Scholarship
— she is the first recipient as the award was established in 2019. “My immediate response
was, ‘Are you sure?’ There were so many students deserving of this award,” she said.
2019 TTUHSC Clinical Research Institute Medical Student Award for Outstanding Scholarship
— she is the first recipient as the award was established in 2019. “My immediate response
was, ‘Are you sure?’ There were so many students deserving of this award,” she said.
Gavin won the award for her research work in ulcerative colitis. She is currently completing her general surgery rotation at TTUHSC after completing two dermatology rotations at the University of Texas Medical Branch Health Hospital and the University of Tennessee College of Medicine respectively.
Three-Dimentional Vision Proves True
Recently appointed chair of the Department of Obstetrics and Gynecology in the Permian Basin Tried to Prove Robots Wrong
Michael Galloway, DO, pursued robotic surgical training for one reason: to prove  it wasn’t as good as traditional methods. The attendings at Wright State Physicians
Women’s Healthcare in Dayton, Ohio, were using the robotic systems for gynecological
surgeries, causing residents to miss out since they weren’t trained to use the equipment.
Galloway, who considered robotics to be a “fancy new car” everyone was chasing, found
himself backtracking after his residency training. Robotic surgery had many benefits
to the patient — shorter recovery time and hospital stay — but also to the surgeon
— less physical toll and decreased margin of error.
it wasn’t as good as traditional methods. The attendings at Wright State Physicians
Women’s Healthcare in Dayton, Ohio, were using the robotic systems for gynecological
surgeries, causing residents to miss out since they weren’t trained to use the equipment.
Galloway, who considered robotics to be a “fancy new car” everyone was chasing, found
himself backtracking after his residency training. Robotic surgery had many benefits
to the patient — shorter recovery time and hospital stay — but also to the surgeon
— less physical toll and decreased margin of error.
A passionate educator, Galloway struck a deal with the attendings: if he trained his residents in robotic surgery, they could assist the attendings. Finding an outdated robotic system in a closet while serving as the director of the obstetrics and gynecology program at Wright State University, he renamed the storage room the Residency Robotic Training Center and got to work.
In comparison to laparoscopic surgery, robotic systems had two lenses for multidimensional perspective, and when you moved the lever to the left, the instrument goes to the left, whereas laparoscopic implemented the fulcrum effect — you move the lever to the left, the instrument goes to the right.
Over the next 12 years, he would build a state-of-the-art robotic residency training facility. What started as a pipe dream he’d sketched out on a napkin, became a renowned training program where residents walked away with a well-rounded education in robotic vaginal and abdominal surgeries.
“I want my residents to be competitive as well as be able to serve the patients’ needs,” he said. “And it’s hard to do that if you can only perform one type of surgery.”
Gary Ventolini, MD, School of Medicine dean in the Permian Basin was on faculty at Wright State University from 2005 to 2012 and had been watching Galloway’s residency program. When Moss Hampton, MD, retired in January 2019, Ventolini reached out to Galloway.
Galloway joined TTUHSC in July, moving 1,300 miles to serve as professor and chair of the Department of Obstetrics and Gynecology and as director of the OB/GYN residency program in the Permian Basin. Galloway hopes to strengthen the gynecology side of the department and incorporate robotics into surgical training. Based on his previous track record, we can expect positive changes through the lens of what is in the best interest of both patients and residents.
Graduate School of Biomedical Sciences
PhD Candidate is the First TTUHSC Student to Receive F31 NIH Grant
Get to Know Brianyell McDaniel Mims
Brianyell McDaniel Mims had one question for her college adviser: “What are my  career choices?”
career choices?”
She enjoyed science and had chosen a major in biochemistry. Her adviser helped her apply for the RISE (Research in Science and Engineering) program, which gave Mims an opportunity to work in a science laboratory. “I had no idea I could have a career in science, and once I started working in the lab, I knew I wanted to do this for the rest of my life,” Mims said.
When considering higher education options after graduation, she decided to interview at TTUHSC, though apprehensively.
“I was nervous because I felt like I was the only black face when I arrived,” she said. “I was afraid I was going to be treated differently, which I was, but it wasn’t the way I expected. Everyone was so friendly and were very familiar with me as an individual and knew the little things about me. When Dr. Grisham found out I was from New Orleans, he said he’d love to have me in his lab since we’re both from Louisiana!”
Almost four years later, and Mims is the first TTUHSC PhD candidate to receive a NIH F31 Pre-Doctoral Fellowship Award — estimated at $91,500 over a three-year period – for her work in the role of T cells and the intestinal microbiota in mouse models of acute graft versus host disease. Patients diagnosed with cancer, blood disorders and autoimmune diseases qualify to receive stem cell transplantation for treatment. However, a 100% perfect match is rare, which can cause many patients receiving stem cell transplants to contract acute graft versus host disease. This disease manifests in inflammation of multiple organs.
“You treat one disease, yet cause another,” Mims added. “The cancer or blood disorder is gone but now you have acute graft versus host because the stem cells that are transplanted are attacking the different tissues in the body, which can lead to multiple organ inflammation.”
Additionally, the radiation that patients receive before transplantation can be damaging to body tissues, especially the gut. Mims’ work revolves around manipulating T cells in mouse models of acute graft versus host disease in the absence of toxic pre-conditioning such as radiation and intestinal injury.
Mims is expected to graduate in May 2020 with her PhD in Biomedical Sciences: Immunology and Infectious Diseases.
Get to Know Brianyell McDaniel Mims:
- One of eight siblings.
- First-generation college student. One of the first of 44 grandchildren to attend college.
- Loves vampire novels.
- Dancer in high school and college.
- Interest in science peaked in 2009 during the swine flu pandemic after scientists created a vaccine.
- Applied to several graduate programs alongside her cousin, Myeisha McDaniels. “We did literally everything together, and graduate school was no exception. Myeisha was murdered in New Orleans in January 2016 right before the interview process began. Now everything that I do is for the both of us. She is my motivation.”
Top Three Things To Know About Ovarian Cancer
1. It’s aggressive and hard to prevent.
Options for prevention such as screenings and exams are all but nonexistent for ovarian
cancer. There are few symptoms, other than cramping, making early diagnosis difficult.
A patient with ovarian cancer is likely to already be in stage three or four of the
disease upon diagnosis.
2. It responds well to chemotherapy, at first.
The cancerous tumors on fallopian tubes or ovaries generally respond well to therapy.
“However, in more than 70% of patients in remission, there is re-occurrence,” said
Komaraiah Palle, PhD, associate professor in the Department of Biotechnology. Dormant
cancer cells do not respond to chemotherapy. These dormant cancer cells then become
active and are now therapy-resistant, leading to high percentages of ovarian cancer
fatalities.
3. Extramural funding supports search for solutions.
Palle received a $200,000 grant from the Cancer Prevention and Research Institute
of Texas to treat both active and dormant cancerous cells simultaneously to prevent
re-occurrences of this deadly disease. “We’ve found a protein target and small compound
inhibitors, that, when combined with chemotherapy, should accomplish this goal. Research
is ongoing.”
Jerry H. Hodge School of Pharmacy
Standing-Room-Only Opportunity
During the West African Ebola outbreak (March 2014 to June 2016), more than 28,000 cases of the highly contagious and fatal virus were reported to the World Health Organization – about 39% of those, or 11,308, resulted in deaths. People in Liberia, a fragile nation due to years of civil unrest and poor public health infrastructure, were among those most affected.
In 2019 and 2018, Whit Walker Jr., MD, assistant professor of internal medicine in
Amarillo, traveled to Liberia with Samaritan’s Purse International Relief to teach
family medicine residents about Ebola and its treatment. Working with the global humanitarian
organization, Walker’s teaching audience took a slightly different turn on his 2019
trip — he also began teaching Liberian pharmacy students about Ebola and other illnesses
prevalent in the area.
“During a rotation with residents, three pharmacy students asked if they could join
us,” Walker said. “I scheduled a lecture thinking only these three would attend. Ten
came. They were eager to learn.”
The students impressed Walker, and he wanted to do more upon his return to Amarillo. Walker collaborated with Jill Frost, PharmD, associate professor in the Jerry H. Hodge School of Pharmacy, students and other faculty to create an online lecture series. Now, every two weeks, Walker, along with faculty and students reach across the globe to a room full of aspiring pharmacy students in Liberia where, oftentimes, it’s standing room only.
The Liberian students aren’t the only ones learning, said Rachel Bassinger, PharmD, assistant professor in the Jerry H. Hodge School of Pharmacy. “This experience is very eye-opening for our students. Not only are they sharing what we do in the states, but they are becoming more culturally aware. They see how motivated the Liberians are to learn, in spite of the obstacles in their way.”
Vaping on the Brain
What was meant to be a healthier alternative to smoking has now claimed the lives of at least 10 people in the U.S. and sickened more than 400. And experts can’t figure out why.
Scientists in the Jerry H. Hodge School of Pharmacy are studying the effects of long-term vaping on the brain. Thomas Abbruscato, PhD, Luca Cucullo, PhD, were awarded a three-year $1.36 million grant from the Food and Drug Administration through the National Institute on Drug Abuse for their study, “Blood and Brain Based Biomarkers of Injury to Assess the Cerebrovascular Impact of Emerging Alternatives to Classic Cigarette Products.”

